This article was last updated on January 4, 2026.
Your best underwriter processes medical histories significantly faster than newer staff. She spots red flags in lab reports that others miss. She knows which physician notes matter for risk assessment and which prescription patterns indicate emerging conditions. But her pattern recognition, risk assessment shortcuts, and exception handling live in her head, not in a playbook your entire team can execute.
Insurance operations teams seeking to automate medical records review face a growing volume challenge. Lab reports, physician notes, prescription histories, and imaging summaries each require manual extraction, cross-referencing, and data entry into policy systems. Claims adjusters wade through stacks of treatment documentation, hunting for the specific clinical details that determine coverage decisions.
Automating medical records review scales your best reviewers' approach across every case. Here's how insurance operations teams are making the transition from manual processing to AI-assisted workflows.
Why Reviewing Medical Records Manually Breaks Down
Medical records arrive in every format imaginable. Faxed physician notes with illegible handwriting, scanned PDFs from hospital systems, and structured lab reports mixed with free-text clinical summaries all require different extraction approaches. The same information appears in different locations depending on the source.
Manual medical records review breaks down across several dimensions:
- High operational costs: Claims adjudication represents a significant portion of operational costs, with much of that spending tied to potentially avoidable inefficiencies from manual data extraction, repeated review cycles, and errors that trigger denials
- Denial rates that indicate process failure: Many denials are overturned on appeal, indicating initial review processes are failing at concerning rates
- Compounding accuracy problems: Errors create cascading inefficiencies, throughput constraints limit how volume scales, and backlogs emerge during peak periods
- Quality variation from temporary staffing: Hiring temporary staff introduces inconsistency, while experienced processors spend time on training rather than production work
- Compliance documentation gaps: Audit trails require documentation of what was reviewed, what was extracted, and how decisions were made, but manual processes make this burdensome, leading to gaps that create regulatory risk
What Medical Records Automation Actually Involves
Automating medical records review requires multiple technologies working together rather than a single tool. The workflow moves through distinct phases, each handling a specific processing challenge.
Automate Document Intake and Classification
Records arrive through provider portals, fax, email attachments, and connections from health information platforms. Automation systems ingest these varied formats, classify document types, and route them to appropriate processing queues. The classification system extracts structured data elements including diagnosis codes, treatment histories, and medication lists.
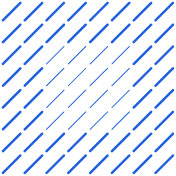
Datagrid's Data Organization Agent ingests and structures data from disparate sources (e.g., lab reports, physician notes, prescription histories, and imaging summaries), creating a centralized knowledge base that executes documented medical records workflows automatically.
Extract and Structure Text from Records
Optical character recognition converts scanned documents into machine-readable text. More advanced intelligent character recognition handles handwritten physician notes, a capability that matters significantly given how much clinical documentation still arrives in handwritten format. Natural language processing then analyzes the extracted text to identify clinical concepts such as diagnoses, procedures, medications, and treatment timelines.
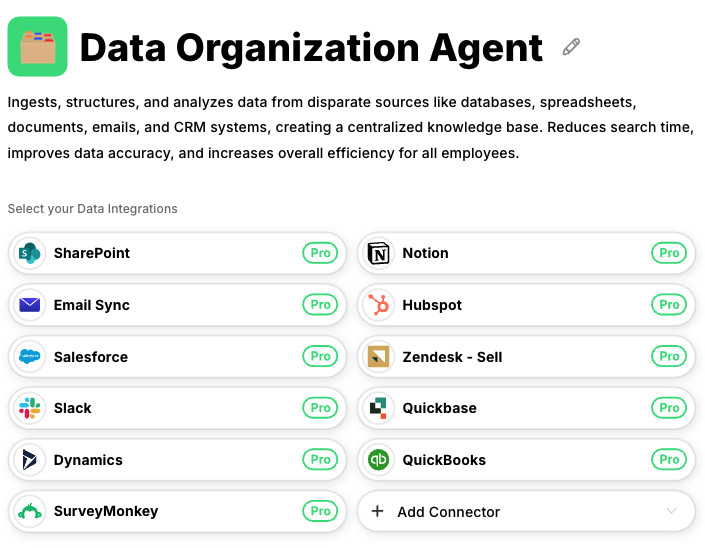
Datagrid's Data Extraction Agent processes varied formats automatically, converting scanned documents and handwritten notes into structured data while applying confidence scoring to flag uncertain extractions.
Route Exceptions with Confidence Scoring
AI agents assess their own extraction confidence for each data point, routing cases to appropriate review tiers based on confidence thresholds.
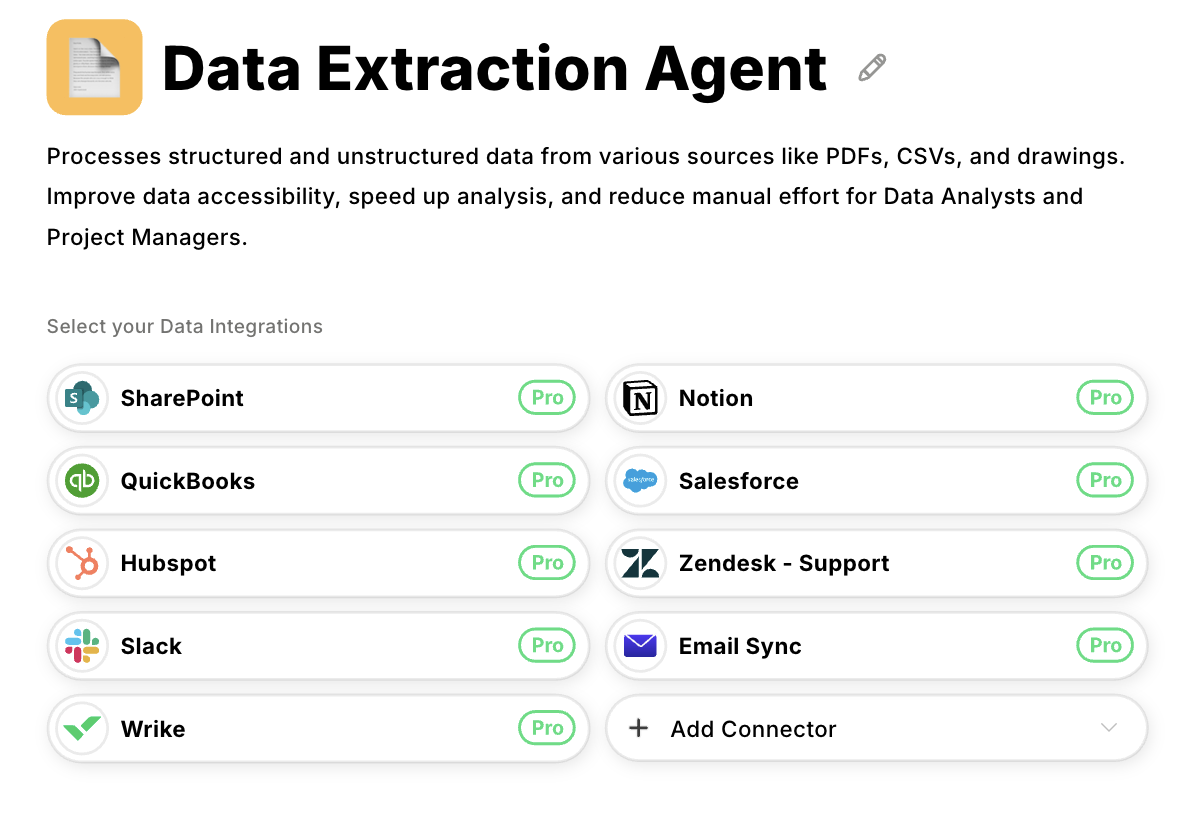
Datagrid's Claims Processing Agent handles tiered routing automatically, processing high-confidence cases through straight-through workflows while escalating exceptions to human reviewers based on predefined confidence thresholds.
Where AI Agents Handle the Work vs. Human Review
The question isn't whether to automate but which workflow steps automation handles best. Research demonstrates that human-AI collaboration models deliver optimal operational results when AI agents handle routine, high-confidence tasks while humans review exceptions.
Tasks Suited for AI Agent Execution
AI agents excel at repetitive, rule-based extraction and validation tasks that consume significant processor time:
- Extracting structured data from standard document formats
- Cross-referencing medication lists against formularies
- Compiling treatment timelines from multiple source documents
- Flagging missing documentation before underwriting review
- Validating data completeness against submission checklists
- Detecting patterns that indicate potential fraud for investigation
Tasks Requiring Human Expert Review
Human experts focus on complex risk assessment requiring specialized medical knowledge, exception handling for low-confidence cases, relationship and strategic functions, fraud investigation, regulatory interpretation, and model validation. Even as AI agents become deeply embedded across underwriting and claims operations, human judgment remains central.
Segment Cases into Tiered Processing
The optimal model segments cases into three tiers. Cases with high confidence scores proceed through straight-through processing without human intervention. Cases scoring in the middle range receive automated processing followed by quick human validation. Cases below established thresholds require full expert review with AI agent support.
The operational impact of this tiered model is measurable. Organizations implementing human-AI collaboration report meaningful processing time reductions depending on document complexity and standardization. Perhaps most significantly for capacity-constrained teams, automation enables processors to handle considerably more records per shift rather than the limited volume typical of manual workflows. This throughput improvement directly addresses capacity constraints without adding headcount.
A Phased Approach to Implementation
Establishing proper data infrastructure and business process foundations before deploying automation is critical to implementation success. Successful deployments follow a phased approach spanning 12-18 months.
Phase 1: Assessment and baseline measurement (Months 1-3). Document current workflows in detail. Map how medical records move through your organization. Measure baseline performance including processing time per record type, error rates by document category, exception rates, and rework cycles.
Phase 2: Pilot deployment (Months 4-6). Deploy automation to a limited scope, perhaps a single product line or claim type with high volume and relatively standardized documentation. Selecting document types with the highest volume and most standardized formats makes ideal pilot candidates, as they demonstrate clear ROI while minimizing implementation complexity. Target strong accuracy benchmarks before expanding.
Phase 3: Scaled rollout (Months 7-12). Expand incrementally across additional product lines and claim types. Monitor quality metrics continuously for any degradation as volume increases.
Phase 4: Full production and optimization (Months 13-18). Complete rollout across all applicable workflows. Implement continuous quality monitoring dashboards. Establish feedback loops where human reviewer corrections improve AI agent accuracy over time.
A critical success factor involves establishing comprehensive data infrastructure before scaling automation. Organizations that deploy automation without first establishing data foundations experience significantly degraded performance during scaling.
Compliance Requirements You Cannot Ignore for Automated Medical Records Review
Medical records automation in insurance operates under multiple regulatory frameworks that directly impact system design.
HIPAA Business Associate obligations apply to any vendor processing protected health information. Automated systems must maintain comprehensive audit trails capturing every access, extraction, and decision. Organizations must retain audit trail records and compliance-related documentation for a minimum of six years, regardless of how long the underlying medical records themselves are kept.
Audit trail specifics matter. Logs must capture user identification for every access, timestamps, type of access performed, and unsuccessful authorization attempts. For automated systems, this extends to documenting which algorithms accessed which records and what decision pathways led to each determination.
AI governance requirements are expanding rapidly. The National Association of Insurance Commissioners' Model Bulletin on AI use has been enacted in 24 states as of late 2024, with additional states enacting related regulations. These regulations require documented AI programs covering data sources, model architecture, training methodologies, and decision logic. Bias testing protocols and human oversight procedures are mandatory components.
Building compliance monitoring into automation architecture from inception supports both regulatory requirements and operational efficiency during deployment.
Scale Your Medical Records Review with Datagrid
Datagrid's AI agents automate the medical records review workflows that consume your operations team's capacity:
- Multiformat document ingestion: Datagrid's Data Organization Agent ingests lab reports, physician notes, prescription histories, and imaging summaries from disparate sources, structuring them into a centralized knowledge base without manual data entry.
- Intelligent text extraction: The Data Extraction Agent processes scanned documents and handwritten clinical notes automatically, converting unstructured records into structured data with confidence scoring that flags uncertain extractions for review.
- Tiered exception routing: The Claims Processing Agent routes high-confidence cases through straight-through processing while escalating complex cases to human reviewers based on predefined thresholds, ensuring expert attention goes where it matters.
- Compliance-ready audit trails: Every extraction, access, and decision is documented automatically, supporting HIPAA requirements and emerging AI governance regulations without adding manual documentation burden.
- Continuous accuracy improvement: Feedback loops capture human reviewer corrections and apply them to improve AI agent performance over time, building institutional knowledge into your automation.
Create a free Datagrid account to start automating medical records review across your insurance operations.